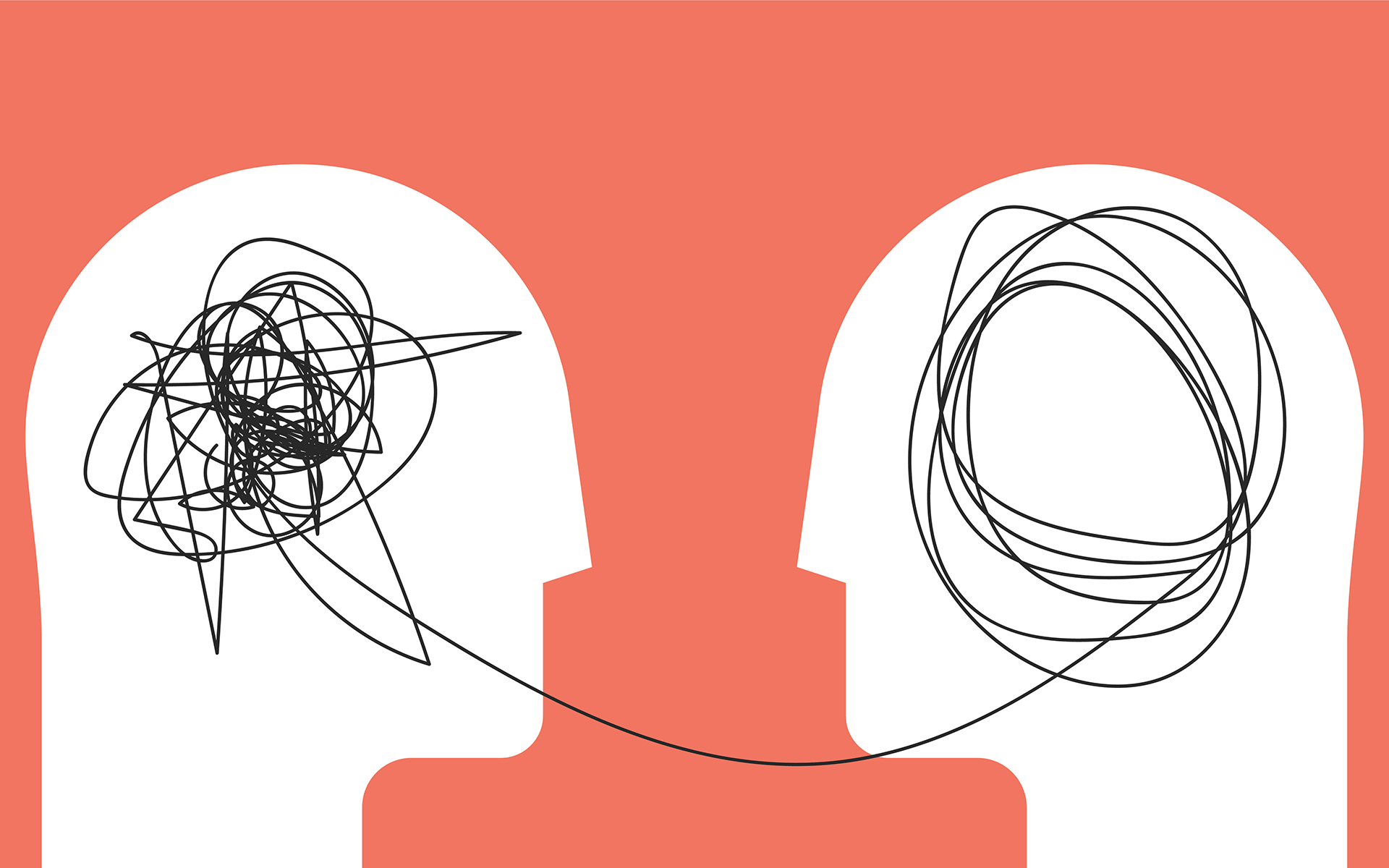
Mindfulness-based cognitive therapies have become increasingly popular for lessening depression. How these treatments work is not fully understood, however. A new study from the Netherlands examined whether the interplay between self-compassion and mood during an eight-week mindfulness program might explain some of these effects.
The study included 118 adults with recurring episodes of depression who had previously participated in Mindfulness-Based Cognitive Therapy. Each was assigned to either a treatment-as-usual waitlist group, or a mindfulness plus treatment-as-usual group.
The treatment-as-usual group received medication and/or psychotherapy, but not any form of compassion-focused intervention. They were given the opportunity to attend mindfulness classes after the first mindfulness group completed their program. The mindfulness group attended eight bi-weekly sessions for two-and-a-half hours in groups of 8-10 people. Much of the program focused on practicing befriending self and others. Individuals were given a CD containing a 30-minute guided meditation and asked to practice daily. They also received written materials covering each session and related practices. Individuals continued to receive medication and/or psychotherapy as needed.
The self-compassion scale measured a number of individual dimensions of experience, like self-kindness: “When I’m going through a very hard time, I give myself the caring and tenderness I need.”
Prior to each session, only the mindfulness group participants completed a questionnaire regarding self-compassion and mood. The self-compassion scale measured a number of individual dimensions of experience, like self-kindness (“When I’m going through a very hard time, I give myself the caring and tenderness I need”) and self-judgment (“I’m disapproving and judgmental about my own flaws and inadequacies”), to more social factors such as “common humanity” (“I try to see my failings as part of the human condition”). Questionnaire items examining negative mood included being “upset” and “scared,” whereas positive emotions included “active” and “excited.”
Some Kind of Good Mood
Results showed an increase in self-compassion over the eight-week intervention. Participant reports of higher levels of self-compassion at the start of each session also predicted lower levels of negative mood the following session. No relationship between self-compassion and positive mood from one session to the next was detected.
These findings differ from previous studies linking self-compassion to improved positive mood. The present study’s authors believe that their use of energetic positive mood states such as “active” and “excited” may explain this difference. During the mindfulness-based treatment, participants are “invited to soothe [themselves] in difficult times, promoting feelings of relaxation, connectedness, safety and wellbeing,” they note. Measuring active positive states may have prevented them from detecting more subtle forms of positive mood like contentment.
Overall, this study suggests that self-compassion focused interventions for those with recurring depression may boost feelings of kindness toward self and others, and lessen negative mood over time. This adds to the growing list of studies finding that mindfulness-approaches may be beneficial for improving mood and human connection, and lessening depressive symptoms.
read more
Q&A: How Mindfulness-Based Cognitive Therapy Can Reach Many More People in Need
Zindel Segal and Sona Dimidjian share the story of their mission to bring MBCT online, and how that led to their new digital platform Mindful Noggin.
Read More
3 Ways to Be Kind to Yourself When You’re Feeling Blue
Feeling unwell can be hard work sometimes—and that might be a sign that it’s time to stop trying so hard. Taking the mindful path means making room for suffering, too.
Read More
Is Mindfulness a Treatment for Depression?
Learning what type of depression you have is the key to successful treatment. Experts advise on when mindfulness can (and can’t) help treat depression.
Read More